Israel’s current health indicators are potentially quite good, but they reflect past investments in the healthcare system. Today, there are signs of a worsening in the relative health of Israel’s population, and the situation is likely to deteriorate further unless there is an increase in the share of state funding, in the overall level of health funding, and in the regulation of the system’s public-private mix.
Israel’s current health indices
The health of Israel’s population looks good by common health metrics like infant mortality and life expectancy at birth. Nevertheless, there are concerning indications for the future.
- Infant mortality is low in Israel at 3.1 per thousand births. This is even low compared with healthcare systems similar to Israel’s in Belgium, German, the Netherlands, France and Switzerland. However, infant mortality has stabilized since 2013, which is worrisome as there is potential for still further improvement among certain population groups.
- Life expectancy at birth is relatively high at 82.5 years, but there are signs that, in terms of life expectancy and years of healthy life, Israel’s relative status is liable to decline.
The financing of Israel’s healthcare system
Israel’s healthcare expenditure as a share of GDP remained relatively stagnant despite the country’s impressive economic growth and, in international comparison, the share of public spending out of total healthcare spending in Israel is relatively low compared with all systems with universal coverage amongst developed nations.
- The share of national expenditure on health out of Israel’s GDP was about 7.4% in 2017, compared to an average of nearly 9% in the OECD and 11% in European countries with health systems similar to Israel’s.
- The share of public expenditure out of total expenditure on health stands at about 63% in Israel, compared to 73.5% in the OECD, and 78% among countries with similar systems. Meanwhile, the share of healthcare spending out of household disposable income rose from 3.9% in 1997 to 5.9% in 2016.
- Between 1995 and 2017, per capita health expenditure in OECD countries has increased on average by 2.6 times, and in countries with health systems that are similar to Israel’s, they have increased by 2.7 times. In Israel, however, per capita health expenditure only doubled over the same period.
- Growth in health expenditure was similar to the growth in GDP per capita – about 1.7% a year, on average, since 1995. However, when taking into account changes in healthcare prices relative to the Consumer Price Index and increased needs rooted in changes in the age structure of Israel’s population, the growth was only 0.9% per age-adjusted standardized person.

Problems in the healthcare system: The public-private mix and physician wages
The relatively low level of public funding and the rising share of private health funding increases health costs and widens gaps in the accessibility of medical services for various population groups in Israel.
The relative increase in health prices is high, and stems, at least in part, from the public-private mix that has developed in the system, and the effect it has on physicians’ wages. Physicians’ wages rose by about 42% between 2011 and 2017, compared to an increase of about 15% among other salaried employees in Israel. One main reason for this is that doctors can refer patients from the public system to their own services in the private system, where they can charge higher prices for treatments that could largely be administered through the public system as well. At the same time, this phenomenon means that doctors are spending less time working in the public system. Therefore, publicly funded institutions compete for their own personnel in the privately paid institutions. This drives pay up in the public system as well.
Israel can improve the state of its healthcare system by employing existing models (already in effect in various countries) of either separating the two systems or unifying regulations across them.
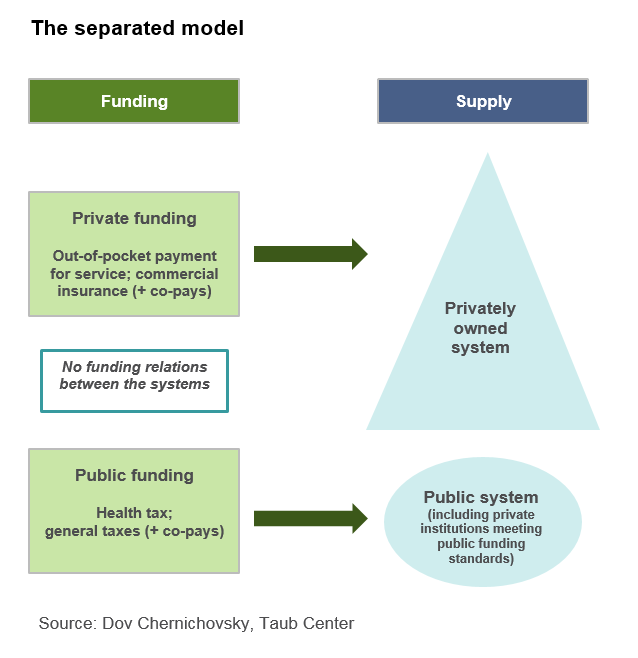
The separated model
In this solution, the two systems would exist at separate funding and infrastructure levels. In the model:
- Public funding would comprise the regular health tax and payments currently transferred to the health funds plus collections for supplementary insurance. Thus, the public framework would also offer the option of choosing a broader healthcare basket than the basic one.
- Any institutions that have contracts for supplying entitled care, and thus funding from the state, would be considered “public,” regardless of ownership, and could compete for publicly funded patients. However, they would have to meet specific criteria to receive public funding.
- In the private system, citizens could pay for treatment through a variety of commercial insurance policies or out of their own pockets.
- All patients would have to decide to receive their care in the public or private system before seeking treatment, and this choice would obligate them throughout the course of treatment.
- Healthcare workers whose income is based on public funding would not offer private treatment, but be “full timers” in the publicly funded system.
- Emergency services currently provided by the public system would not support the private system.
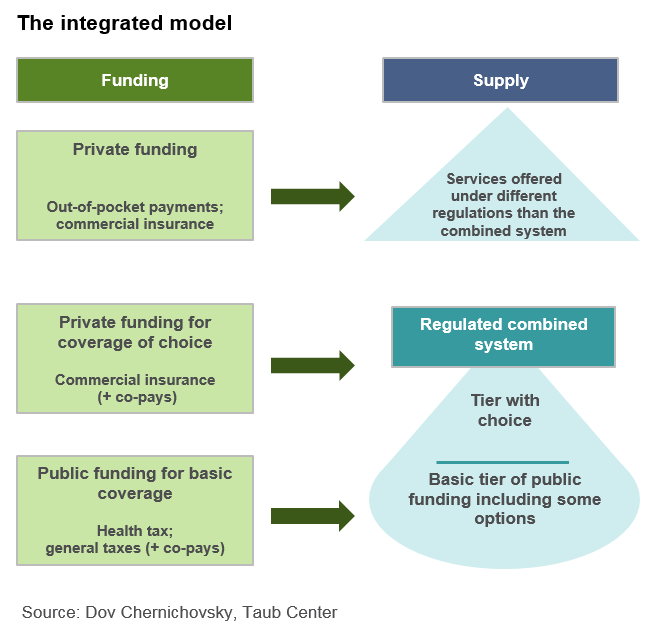
The integrated model
In this solution, the private and public systems would be merged. In the model:
- Every resident would receive basic public insurance, combining today’s basic and supplementary coverages (as in the separated model).
- Another insurance tier would be based entirely on private funding.
- The “integration” comes from the fact that elective services (supplementary and commercial insurance tiers) would be provided as part of the same system that delivers the public services. The extra insurance would be for extra services but not for faster elective service. In essence, the public system would offer a publicly-funded basket and a certain degree of private choice, and public services would be received in both privately and publicly owned institutions, but residents could also pay out of pocket or through insurance for treatments not included in the integrated system.