The first wave of the spread of coronavirus in Israel has, in many respects, been viewed as a success. Compared to other OECD countries, the number of infections per capita in Israel after the first two months of the outbreak has been relatively low, falling well short of countries like Spain, Belgium, Italy, and the US. However, reference group matters. As of May 12, 21 (of 38) developed countries had a lower per capita infection rate than Israel, placing Israel squarely below average of the developed-country pack.
Where Israel has proven more successful is in its low number of COVID-19 deaths. Its (per capita) mortality rates are lower than any country in North America, Western Europe or Scandinavia, including Germany, Finland and Iceland – whose responses to the pandemic have all been praised in the international media. Here, too, however, reference group matters. Israel’s mortality rate is still higher than 13 other developed countries, all of which are in Eastern Europe, Asia or Australasia.
Over time, the growth in confirmed coronavirus cases in Israel began to slow: while the growth was in the 20%-30% range during March, by early April it declined below 10%. By early May it had fallen below 1%, and by May 10 below 0.2% per day.
Another positive sign is that, while during March the percentage of people testing positive for coronavirus increased alongside the number of tests, in April the number of tests continued to climb, but the percentage of people testing positive declined. Since mid-April, there has also been a decline in “active cases” in Israel (all cases that have not yet resulted in recovery or death) and the ratio between new confirmed cases and recoveries flipped such that there are now about 10 recoveries for each new confirmed case.
These trends are not being experienced equally across the country. Throughout April, the most rapid increases in the infection rate took place in seven Haredi (ultra-Orthodox) towns and in the three large mixed Haredi/non-Haredi cities: Jerusalem, Bet Shemesh, and Tzfat.
In our estimates—based on Ministry of Health information—we have shown that although the seven Haredi towns are inhabited by only about 5% of the national population, they accounted for 23% of all new infections nationally between March 31 and May 12. A further 32% of all new infections nationally came from the three mixed Haredi/non-Haredi cities, which contain less than 14% of the national population.
Taking a look at the overall picture, Israel has been relatively successful thus far in its public health response to the coronavirus. What are the factors that have driven these outcomes? In terms of the preparedness of Israel’s hospital system, the situation is complex. Israel falls below the OECD average on some key medical resources including curative hospital beds and nurses per capita.
However, at the same time, Israel has a relatively high number of doctors per capita. Israel also put in early and strict closures and quarantine restrictions which, though not immediately enforced everywhere, contributed to stemming the spread of the virus. In this regard, Israel was helped by the fact that it is a small, centralized country with non-fluid borders. It shares this advantage with other “good” performers like New Zealand, Australia, Iceland, Taiwan, and South Korea.
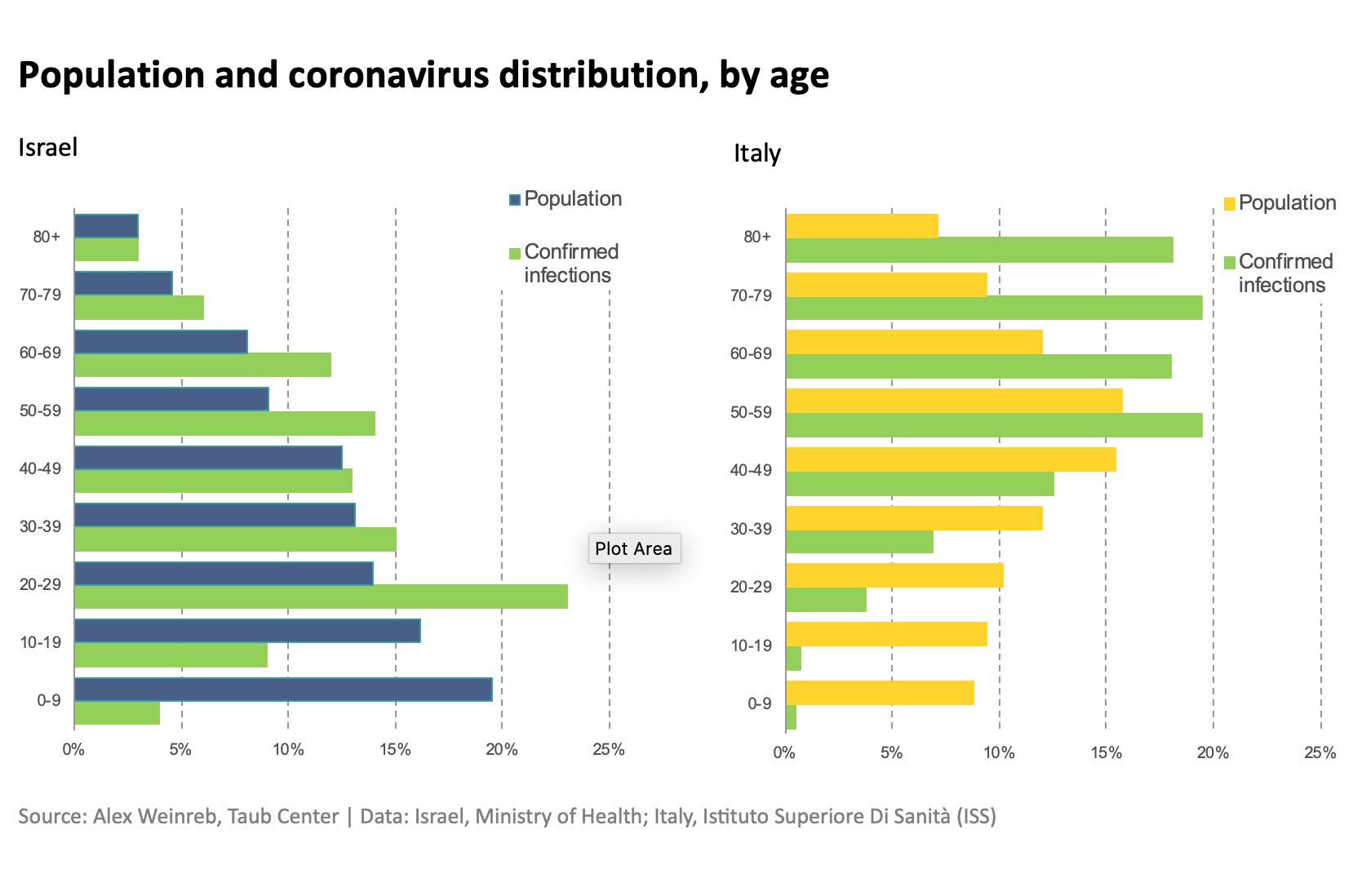
Another factor in explaining Israel’s relative success is its “demographic good fortune.” As we see around the world, mortality from COVID-19 is higher among the elderly (a fact that is not historically true for all epidemics; for example, the Spanish Influenza outbreak, around the end of WWI, disproportionately killed people between their teens and age 40). The first element of Israel’s good fortune is that its population is relatively young: those ages 65 and older make up about 10% of the population, compared to about 23% in Italy and about 17% in the U.S.
The second aspect of Israel’s good fortune is that the infection in Israel has disproportionately spread among the young – particularly the 20-29 age group. In Italy, by contrast, the population is not only generally older, but coronavirus infections also disproportionately spread among the elderly.
Finally, the unintended consequences of Israel’s other country characteristics, even beyond its small size and relative isolation, might contribute to Israel’s success. For example, a major risk factor for mortality from COVID-19 is cardiovascular disease. Yet Israel has much lower mortality from cardiovascular disease than the U.S. and other developed countries.
Furthermore, the additional resources and quick mobility of Israel’s security forces and a population familiar with times of national struggle, as well as institutional nimbleness and skilled professionals in a variety of fields, have helped to bolster the country’s response to the coronavirus outbreak.
Much of the coronavirus response is still ahead of us. However, it seems that in Israel, at least, some combination of planning and responsive policy, the age structure of the population and those infected, and other country characteristics, has allowed it to come out of the first couple of months of the outbreak in a relatively good position.